Stroke: First evidence of effective therapy for severe cerebral hemorrhage
Bleeding in deep areas of the brain is usually life-threatening / Little therapeutic progress to date / International team led by the Medical Center - University of Freiburg finds first evidence of positive effect of temporary skull opening
More than 50,000 people in Germany suffer a spontaneous hemorrhage in the brain every year. Such a hemorrhagic or bleeding stroke is acutely life-threatening. Bleeding deep in the brain in particular usually has massive consequences. The bleeding and subsequent swelling exert pressure on the surrounding brain tissue, causing extensive damage to the brain. There has been no effective therapy to date. Now, for the first time, there are valuable indications of an effective neurosurgical approach, as shown by an international team of physicians from the University Hospitals of Fribourg and Bern, Switzerland. They found evidence that opening the skull and thus reducing the pressure in the brain leads to less severe courses of the disease The so-called SWITCH study was published on 15 May 2024 in the leading specialist journal The Lancet and was presented at the same time at the European Stroke Organization (ESOC) congress in Basel.
"This study is the culmination of 14 years of hard work and passion," says Prof. Dr. Jürgen Beck, Medical Director of the Department of Neurosurgery at the Medical Center - University of Freiburg. He led the study together with Prof. Dr. Urs Fischer from Inselspital at Bern University Hospital, Switzerland. "The SWITCH study is the first to provide strong evidence for an effective therapeutic approach to deep hemorrhagic stroke. In the future, the focus will be on applying the results to individual patients."
Deep-seated hemorrhages are particularly dangerous
Bleeding in deep-seated regions of the brain is particularly dangerous for patients. They often lead to severe disabilities, the need for care and a high mortality rate. Treatment options are currently limited to antihypertensive and hemostatic drugs and are often inadequate - there is no therapy that has been proven effective by studies. At the same time, research into deep brain haemorrhages is particularly challenging, as the affected areas of the brain are difficult to access and bleeding can quickly become life-threatening. Previous studies on various surgical methods have failed to show a clear benefit for patients.
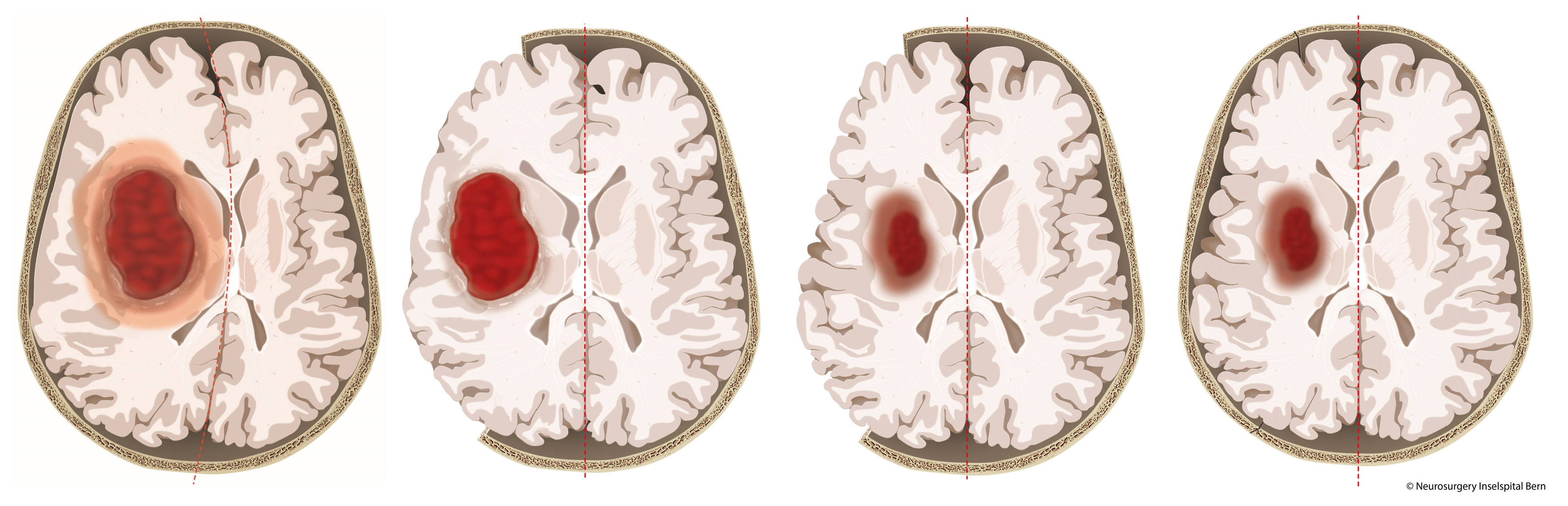
The SWITCH study therefore specifically investigated the effect of a craniectomy to relieve pressure in particularly severely affected patients. Part of the skullcap was removed and reimplanted once the swelling had subsided. The patients received either the previous standard therapy or the standard therapy in combination with the decompression craniectomy.
Results give hope - further research needed
The SWITCH study enrolled 197 participants over 9.5 years, all of whom had a severe deep-seated hemorrhagic stroke. The patients were aged between 18 and 75 and on average 61 years old. The treatment took place in 42 stroke centers in Austria, Belgium, Finland, France, Germany, the Netherlands, Spain, Sweden and Switzerland. Due to funding running out, the original study target of 300 participants could not be achieved. The effects were evaluated in particular using an established scale for neurological assessment after a sleep attack, the modified Rankin Scale from 0 (no complaints) to six (death).
Six months after the procedure, 44 percent of patients were assigned to the worst levels 5-6 after combination therapy, compared to 58 percent without neurosurgery. Negative effects occurred equally frequently in the groups. Even if statistical significance (p=0.057) was narrowly missed, the authors still see this as weak evidence that the intervention could be superior to the previous therapy. "It is a valuable glimmer of hope that the intervention can alleviate the suffering of these patients," says Beck. However, survival and severe disability were high in both groups, so further research is needed.
Risk factors and signs
Typical risk factors for a hemorrhagic stroke are high blood pressure and the use of blood-thinning medication. Alcohol consumption and smoking also increase the risk.
The signs of a hemorrhagic stroke depend on the region of the brain affected. Typical symptoms are
- sudden, one-sided muscle weakness in the arm, leg and face
- loss of balance
- slurred speech
- nausea, vomiting, drowsiness and loss of consciousness.
If a stroke is suspected, the emergency services must be called immediately on 112.
Original title of the study: Decompressive craniectomy plus best medical treatment versus best medical treatment alone for spontaneous severe deep supratentorial intracerebral haemorrhage: a randomized controlled clinical trial. The Lancet. 2024
DOI: 10.1016/S0140-6736(24)00702-5
Link to the study:https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(24)00702-5/fulltext
Caption: To prevent severe pressure damage after a brain hemorrhage, the physicians in the study temporarily removed part of the skull bone. Once the swelling had subsided - usually after a few weeks - the bone was implanted again.
Image source: University Department of Neurosurgery, Inselspital Bern
Back
Medical Center - University of Freiburg
Central Information
Phone: 0761 270-0
info@uniklinik-freiburg.de
For press inquiries:
Corporate Communications
Breisacher Straße 153
79110 Freiburg
Phone: 0761 270-84830
kommunikation@uniklinik-freiburg.de
