Body's own defenses help with esophageal cancer
Immune cells play a central role in treatment success / Study in Nature Cancer shows that changes in the tumor environment are more important than new mutations
In patients with oesophageal cancer, it is not only chemotherapy, but above all the immune system that determines the success of the treatment. This is shown by a recently published study with significant involvement of the University Medical Center Freiburg. The researchers discovered that If the body's own defense cells - especially so-called T cells - remain active, the chance of a successful therapy is significantly higher. If, on the other hand, the immune system appears weakened or blocked, the tumor often responds poorly to treatment. The results were published in the journal Nature Cancer on May 14, 2025.
"Our data show that the reaction of the immune system plays a decisive role in determining how well a therapy works - even if the tumor hardly changes genetically," says co-study leader Prof. Dr. Michael Quante, Head of the Gastrointestinal Tumor Center at the Department of Internal Medicine II at the Freiburg University Medical Center
Tumor remains the same - environment changes
Tissue samples from 27 patients with locally advanced esophageal cancer were examined for the study. All of them had received so-called neoadjuvant therapy - i.e. treatment prior to surgery, usually in the form of chemotherapy or combined radiation-chemotherapy. The results showed that the cancer cells themselves remained surprisingly stable. The changes mainly took place in the environment of the tumor - in the immune cells, the connective tissue and the signaling pathways between cells.
Immune escape as a weak point
What was particularly striking was that in tumors that responded poorly to the therapy, the researchers found evidence of what is known as immune escape. This involves the cancer changing certain surface characteristics so that it is no longer recognized by the immune system. Inhibitory signals such as the PD-L1 molecule were also elevated in these patients - they are considered potential targets for modern immunotherapies.
Prospects for new combination therapies
The study was conducted as part of the MEMORI study, in which several sites of the German Cancer Consortium (DKTK) were involved - including Munich, Freiburg and Essen. A central component of the study was the analysis of tumor evolution under therapy using gene sequencing, which was carried out together with co-study leader Prof. Trevor Graham, Director of the Centre for Evolution and Cancer at the Institute of Cancer Research in London, as part of a Cancer Aid Mildret Scheel Fellowship for Dr. Melissa Barroux.
The results provide important information on how immune responses can be recognized at an early stage and specifically supported in the future - for example through combinations of chemotherapy and immune-activating drugs. The aim is to make therapies for patients with oesophageal cancer more effective and easier to control.
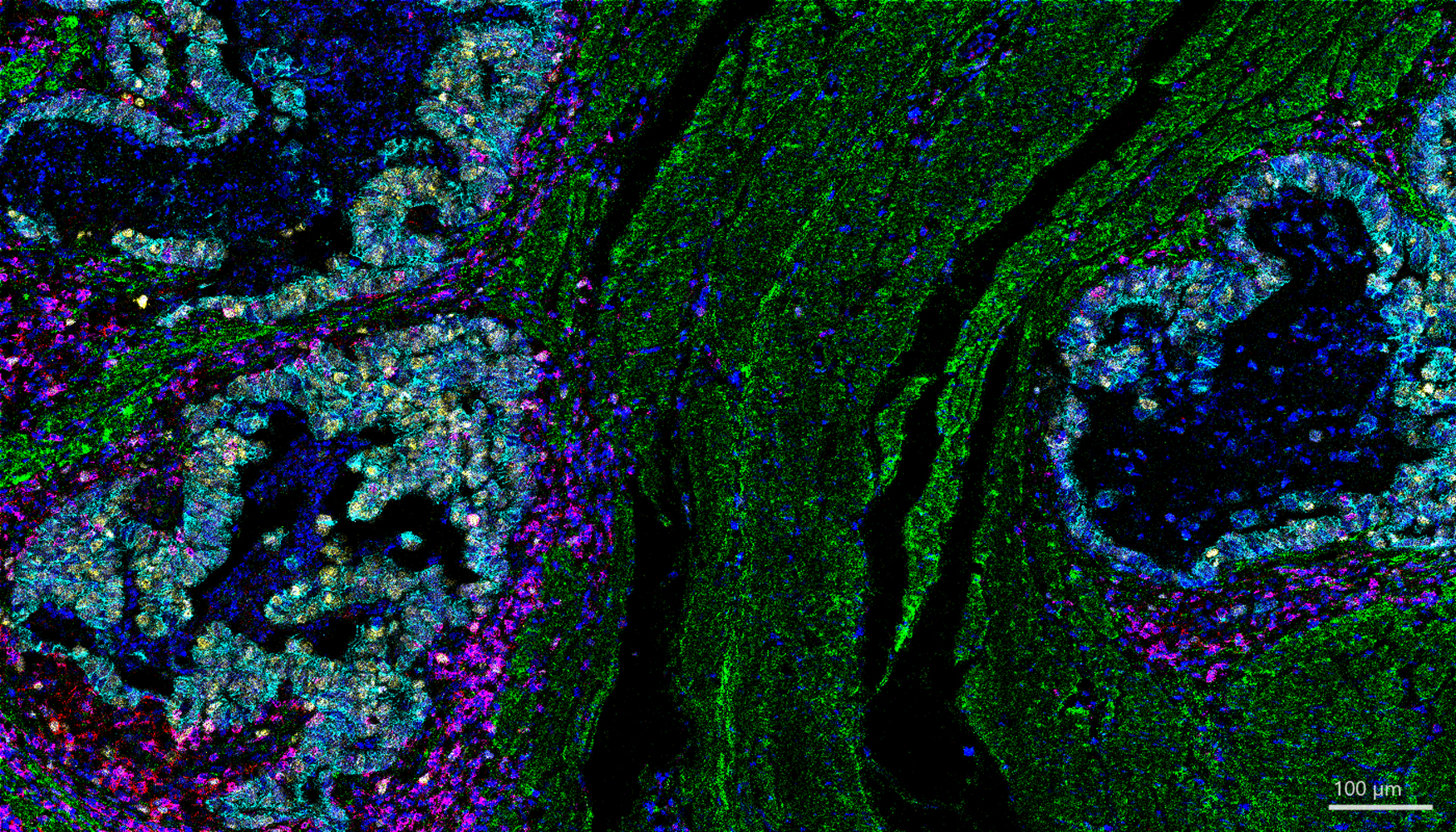
Picture caption: Memory T cells (red) and killer T cells (purple) are together in the immediate vicinity of cancer cells (yellow). These immune cells "know" tumor cells from previous contacts and can fight them quickly and effectively. Green: Connective tissue
Image rights: University Medical Center Freiburg / Bertram Bengsch, Martin Borgmann, Michael Quante
Original title of the publication: Evolutionary and immune microenvironment dynamics during neoadjuvant treatment of esophageal adenocarcinoma
DOI: 10.1038/s43018-025-00955-w
Link to the study:https://www.nature.com/articles/s43018-025-00955-w
Back
Medical Center - University of Freiburg
Central Information
Phone: 0761 270-0
info@uniklinik-freiburg.de
For press inquiries:
Corporate Communications
Breisacher Straße 153
79110 Freiburg
Phone: 0761 270-84830
kommunikation@uniklinik-freiburg.de