Light therapy for immune cells helps with side effects of cancer therapy
A common side effect of cancer immunotherapies can probably be stopped by activating immune cells with light, as researchers at the Medical Center - University of Freiburg show / Publication in the New England Journal of Medicine
It is only in recent years that melanoma, also known as black skin cancer, has been treatable with medication. However, every second patient experiences severe autoimmune reactions such as skin rashes or diarrhea. Researchers at the Medical Center - University of Freiburg and Swiss colleagues have now shown that these can be stopped with special light therapy. They successfully treated a 29-year-old cancer patient with severe inflammation of the intestinal mucosa using extracorporeal photopheresis (ECP). This involves adding a light-reactive drug to immune cells outside the body, irradiating them with UV light and returning them to the body. The procedure is believed to activate immune cells that stop the inflammation. The photopheresis therapy led to a complete resolution of the patient's symptoms, while the ongoing cancer therapy successfully treated the skin cancer. Previous, established treatment approaches had been unsuccessful. The case description was published in the renowned New England Journal of Medicine on January 15, 2020.
"The patient responded incredibly well to our new treatment approach. With extracorporeal photopheresis, we have found an important therapeutic option for him and hopefully for many other patients," says principal investigator Prof. Dr. Robert Zeiser, Head of the Department of Medicine I Specialties: Hematology, Oncology and Stem Cell Transplantation at the Medical Center - University of Freiburg. "In principle, the therapeutic approach is also conceivable for immune-mediated side effects of other cancer therapies," says Zeiser. The effectiveness of ECP was demonstrated by Zeiser's research group in collaboration with Dr. Frank Meiß andProf.Dr. Dagmar von Bubnoff, both senior physicians at the Department of Dermatology and Venereology at the Medical Center - University of Freiburgtogether with Prof. Dr. Burkhard Becher from theInstitute for Experimental Immunology at the University of Zurich.
Replacement for cortisone therapy with many side effects
So-called immune checkpoint inhibitors are used in the treatment of malignant melanoma and many other types of cancer. "Cancer cells often have a kind of cloak that makes them invisible to the body's own immune response. Immune checkpoint inhibitors remove this cloak and enable the immune system to attack the cancer cells," explains Zeiser. However, the immune system often also begins to destroy the body's own structures. These side effects can affect various organs such as the intestines, skin, thyroid gland, liver or brain. "Until now, patients with such side effects of cancer immunotherapy have usually been treated with cortisone or other immunomodulating agents for a longer period of time, but this does not always work or can have severe side effects," says Zeiser. In addition, cortisone is suspected of blocking the immune response to the tumor and thus torpedoing the cancer treatment.
The ECP treatment was repeated in the patient every two to four weeks for eight months. Shortly after the start of the therapy, the severe diarrhea caused by the inflammation completely subsided. As the researchers discovered, a certain type of immune cell became larger and more active during ECP therapy. "We assume that these enlarged immune cells act on other parts of the immune system and thus slow down the inflammation," explains Zeiser. The therapeutic approach also proved to be safe in preclinical animal models. "It was very important for the accompanying therapy that the ECP treatment had no negative influence on the anti-tumor effect of the immune drugs," says Zeiser.
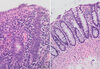
Caption: Before therapy begins, the bowel is inflamed and swollen. Diarrhea is the result. After phototherapy, the condition of the intestine has completely returned to normal.
Difference at cellular level: While the tissue proliferates unstructured before the therapy, the mucus-forming cell clusters are clearly visible again at the end of the therapy.
Image source: The New England Journal of Medicine ©2020
Original title of the publication: Extracorporeal Photopheresis for Colitis Induced by Checkpoint-Inhibitor Therapy
DOI: 10.1056/NEJMc1912274
Link to the study: www.nejm.org/doi/full/10.1056/NEJMc1912274?query=featured_home
Contact:
Prof. Dr. Robert Zeiser
Head of the Department of Tumor Immunology
Department of Medicine I (Specialty: Hematology, Oncology, Stem Cell Transplantation)
Department of Medicine I (Specialties: Hematology, Oncology and Stem Cell Transplantation)
Phone: 0761 270-34580
robert.zeiser@uniklinik-freiburg.de
Back
Medical Center - University of Freiburg
Central Information
Phone: 0761 270-0
info@uniklinik-freiburg.de
For press inquiries:
Corporate Communications
Breisacher Straße 153
79110 Freiburg
Phone: 0761 270-84830
kommunikation@uniklinik-freiburg.de