Muskuloskeletal
Hintergrund
Erkrankungen des Muskel-Skelett-Systems (MSK) sind eine der Hauptursachen für Behinderungen mit hohen individuellen und sozialen Kosten. Traumatische Defekte verschiedener Gelenkstrukturen wie Knorpel, Meniskus oder Bänder können zu einer frühen Arthrose führen. Arthrose ist die häufigste Muskel-Skelett-Erkrankung, deren Prävalenz in unserer alternden Gesellschaft stetig zunimmt.
Die qualitative und quantitative MR-Bildgebung ist ein wichtiges Diagnoseinstrument, mit dem strukturelle Gelenkdefekte und Osteoarthritis frühzeitig erkannt werden können. Die prä- und postoperative MR-Bildgebung nach chirurgischen Eingriffen kann zur Vorhersage und Überwachung des Krankheitsverlaufs und des postoperativen Ergebnisses beitragen.
Die AG MSK arbeitet hauptsächlich an der Entwicklung, Optimierung und klinischen Umsetzung verschiedener qualitativer und quantitativer MR-Sequenzen, um einzelne Gelenkstrukturen nicht-invasiv auf biochemischer und biomechanischer Ebene zu beurteilen.
Forschungsschwerpunkte
Gelenkknorpel
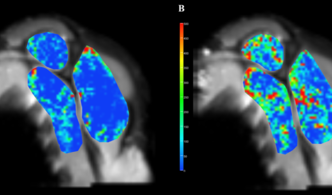
Nicht-invasive Knorpel-MR-Biomarker wie T2-, T2*- oder T1rho-Relaxationszeitmessungen sind in der Lage, frühe biochemische Knorpelmatrixveränderungen zu erkennen, vor allem Erhöhungen des Wassergehalts, Kollagenabbau und Verlust von Proteoglykanen. Es hat sich gezeigt, dass T2-Relaxationszeitmessungen das Fortschreiten des morphologischen Knorpelverlusts vorhersagen können, und sie können einen wichtigen Beitrag zur Beschreibung der Epidemiologie der frühen OA und zur Bewertung der Ergebnisse nach Knorpelreparaturverfahren leisten (Abbildung 1 und 2).
Muskeln
Skelettmuskelvolumen, Fettdegeneration und Durchblutung sind für die ordnungsgemäße Funktion des Bewegungsapparats von wesentlicher Bedeutung. Es hat sich gezeigt, dass qualitative und quantitative Muskel-MR-Parameter mit der klinischen Kraft, dem Fortschreiten der Gelenkdegeneration und den Ergebnissen nach chirurgischen Eingriffen korrelieren (Abbildungen 4 und 5). Möglicherweise können MR-Parameter definiert werden, die die individuelle klinische Entscheidungsfindung im Hinblick auf konservative oder operative Behandlungsstrategien unterstützen.

Metall
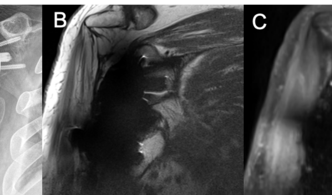
Nach einer Totalendoprothese ist die MR-Bildgebung des periprothetischen Weichgewebes aufgrund der durch das Implantat verursachten großen Suszeptibilitätsartefakte eine Herausforderung. Es wurden Sequenzen zur Reduzierung von Metallartefakten (Slice Encoding for Metal Artifact Correction, SEMAC) entwickelt, um diese Artefakte zu verringern und gleichzeitig die MR-Aufnahmezeit in einem vernünftigen Zeitrahmen zu halten. Diese Sequenzen werden derzeit evaluiert und optimiert, um die periprothetische Beurteilung nach dem endgültigen Gelenkersatz zu verbessern (Abbildung 6). Bei Patienten mit anhaltenden oder neu auftretenden Beschwerden nach einer Totalendoprothese können die zugrunde liegenden Ursachen ermittelt werden. Außerdem ermöglichen diese Sequenzen eine ideale postoperative Nachuntersuchung nach einer Tumorresektion.
Osteoporose
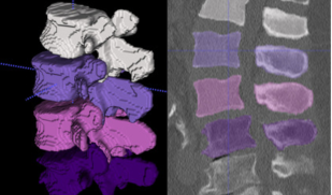
Neue CT- und MR-Bildgebungsverfahren und Nachbearbeitungsalgorithmen ermöglichen eine automatische quantitative Bildanalyse (Abbildung 7). Dies ermöglicht die Osteodensitometrie an der Wirbelsäule in nicht zweckgebundenen Routine-CT-Scans (opportunistisches Osteoporose-Screening) und kann zur Diagnose von Osteoporose beitragen, um eine angemessene Therapie einzuleiten und osteoporotische Frakturen zu verhindern. In Zusammenarbeit mit der Abteilung für Neuroradiologie der Technischen Universität München ([deep-spine.de]deep-spine.de) entwickeln und verwenden wir Deep-Learning-basierte Methoden zur automatischen Bildanalyse.
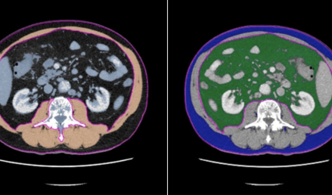
Körperzusammensetzung
CT- und MR-Bildgebungsparameter zur Körperzusammensetzung wie Muskeldichte, Muskelfettanteil (Abbildung 8), Muskelfläche oder Körperfettverteilung stehen Berichten zufolge in Zusammenhang mit Skelettmuskelschwund (z. B. Sarkopenie), Gebrechlichkeit, Krebs, Osteoarthritis und Stoffwechselkrankheiten, einschließlich Diabetes und metabolischem Syndrom. In diesem Zusammenhang können Längsschnittstudien dazu beitragen, die Auswirkungen der Körperzusammensetzung auf die Pathogenese und das Fortschreiten von Krankheiten besser zu verstehen. Darüber hinaus können Analysen der verschiedenen abdominalen Körperkompartimente (subkutanes Fett, viszerales Fett, Bauchmuskeln; Abbildung 9) zur Risikostratifizierung, zur Einleitung von Präventivmaßnahmen und zur Nachbeobachtung während und nach therapeutischen Eingriffen beitragen.
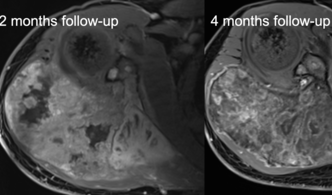
Tumor
Primäre Knochen- und Weichteiltumore sind seltene, aber potenziell tödliche Pathologien, die mittels MR-Bildgebung diagnostiziert werden. Die Ergebnisse nach Bestrahlung, Chemotherapie und/oder Operation von muskuloskelettalen Tumoren unterscheiden sich je nach Tumorentität, pathologischem Grading, Tumorlage und anderen Parametern. Die MR-Bildgebung liefert nicht nur genaue Informationen über die Tumorlokalisation, die Tumorgröße und die beteiligten und infiltrierten Strukturen, sondern kann auch Differentialdiagnosen eingrenzen, die therapeutischen Auswirkungen überwachen (Abbildung 10) und bei der Nachsorge Lokalrezidive erkennen.
| Dr. med. Thierno Diallo (Ansprechperson) |
| Dr. med. Balasz Bogner |
| Dr. med. Matthias Jung |
| Prof. Dr. med. Pia M. Jungmann |
| Dr. med. Dipl.-Ing. Maximilian T. Löffler |
Publikationen
E-Mail Adresse Ansprechperson: thierno.diallo@uniklinik-freiburg.de
E-Mail Adresse für Promotionen: rdia.dissertationen@uniklinik-freiburg.de
Klinik für Diagnostische und Interventionelle Radiologie
Hugstetter Straße 55
79106 Freiburg