Ärzte
Klinisches Bild bei CTLA-4 Defizienz
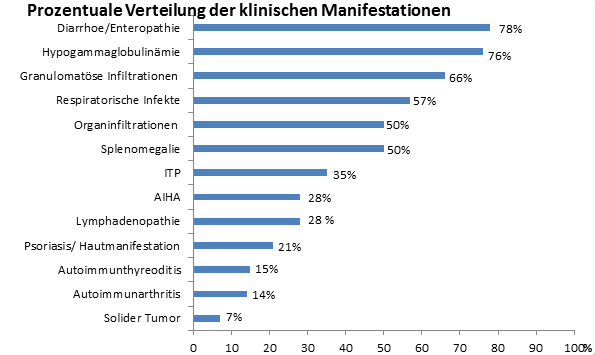
Keimbahnmutationen im CTLA4 Gen stellen einen Risikofaktor für die Entwicklung eines variablen klinischen Bildes eines Immundefekt- und Immundysregulationssyndroms mit Autoimmunität und in den meisten Fällen Hypogammaglobulinämie dar. In ungefähr zwei Dritteln der Patienten zeigt das periphere Blutbild typische Veränderungen eines primären Antikörpermangelsyndroms. Als erste Symptome treten häufig rezidivierende respiratorische Infekte, wie Pneumonien, Bronchitiden und Sinusitiden und schwere Enteropathien mit Gewichts- und Kaliumverlust auf. Ein Teil der Patienten fällt zunächst mit Autoimmunerkrankungen, wie Thombozytopenien oder Autoimmunthyreoditis auf. Die Hypogammaglobulinämie entwickelt sich meist erst im späteren Verlauf. Die Infekte können, müssen aber nicht seit der Kindheit bestehen und werden meist durch virale oder bakterielle Erreger wie Hämophilus influenza und Streptococcus Pneumoniae ausgelöst. Opportunistische Infektionen, wie Tuberkulose oder Aspergillose, sind auch in einigen Fällen beschrieben. Die Infekte haben oft einen schweren Verlauf und können zu Endorganschäden in der Lunge, insbesondere zu Bronchiektasien, führen. Deshalb sollten sie frühzeitig und aggressiv behandelt werden.
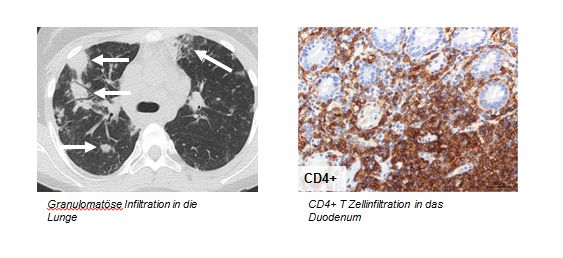
Bei vielen Patienten finden sich entweder granulomatöse Infiltrationen, z.B. im Gehirn oder in der Lunge, oder lymphozytäre Organinfiltrationen vor allem von CD4+ Zellen, insbesondere im Gastrointestinaltrakt, dem Knochenmark, dem Gehirn, den Nieren und der Leber. Diese können zu einer Funktionseinschränkung des jeweiligen Organs, zu Folgeerkrankungen wie einer Nephritis oder, im Falle von Gehirninfiltrationen, zu neurologischen Symptomen führen. In der Lunge findet man häufig eine Kombination der beiden Entitäten in Form einer granulomatösen lymphozytären interstitiellen Lungenerkrankung (GLILD). Darüber hinaus ist bei der CTLA-4 Defizienz das Risiko für Autoimmunerkrankungen, wie Autoimmunzytopenien (ITP, AIHA), -thyreoditis und -arthritis erhöht, häufig entwickeln sich auch Splenomegalien und Lymphadenopathien. Bei den bisher am CCI untersuchten Patienten, traten erste Symptome zwischen dem siebten und 41. Lebensjahr auf.
Immunologischer Phänotyp
Das periphere Blutbild kann Anzeichen eines Antikörpermangelsyndroms aufweisen, wie man es bei Patienten mit CVID (Common Variable Immunodeficiency) findet. Etwa die Hälfte der am CCI untersuchten Patienten wurde mit CVID diagnostiziert bevor die Mutationen in CTLA4 als ursächlicher Krankheitsauslöser identifiziert werden konnte. Bei fast allen Patienten ist eine Erniedrigung der Immunglobulinspiegel in mindestens einer Immunglobulin-Untergruppe zu beobachten. Es besteht meist eine Lymphopenie im peripheren Blut, mit prozentual erhöhtem Anteil CD3+ T-Zellen, erniedrigter prozentueller und absoluter Zahl der CD19+B- und der CD16+CD56+NK-Zellen, sowie einer Verschiebung des Gleichgewichts der CD45RA+ naiven T-Zellen hin zu den CD45RO+ memory T-Zellen. Der CD4/CD8-Quotient ist in der Regel normal, Aktivierungs- und Differenzierungsmarker wie PD1 sind hochreguliert. Außerdem kommt es bei vielen Patienten zu einem progredienten Absinken der Anzahl an CD19+ B-Zellen.
Diagnosestellung
Das klinische und laborchemische Bild bei CTLA-4 Defizienz ist sehr variabel, so dass eine Diagnosestellung auf diese Weise nicht zuverlässig möglich ist. Daher wird die Diagnose in spezialisierten Zentren molekulargenetisch durch den Nachweis der CTLA4 Mutation gestellt. Die Familienanamnese kann bei der Diagnosefindung hilfreich sein. Alle publizierten Fälle mit CTLA-4 Defizienz folgen einem autosomal-dominanten Erbgang – die Wahrscheinlichkeit einer Vererbung der Mutation liegt bei 50%.
Therapie
Das CCI hat in Kooperation mit einer Forschergruppe des National Institute of Health (NIH) in Bethesda, USA ein Therapie-Stufenprotokoll entwickelt, das sich an den individuellen klinischen Manifestationen des Patienten orientiert. Es beinhaltet auf der untersten Ebene eine Antibiotikaprophylaxe und eine Immunglobulinsubstitution. Bei lymphoproliferativen Organinfiltrationen hat sich eine Kombinationstherapie aus mehreren immunsuppresiv wirkenden Medikamenten, wie Prednisolon, Sirolimus, Budesonid und Rituximab als erfolgreich erwiesen. Auch die Therapie mit Abatacept bzw. Belatacept, das die Funktion des körpereigenen CTLA-4 teilweise kompensiert, ist mit vielversprechendem Erfolg durchgeführt worden. Bei Interesse an genaueren Informationen des Protokolls, können Sie uns gerne kontaktieren.

Prof. Dr. med. Bodo Grimbacher
Centrum für Chronische Immundefizienz
UNIVERSITÄTSKLINIKUM FREIBURG
Breisacher Str. 115
79106 Freiburg im Breisgau
Germany
0761 270-77732
0761 270-77744
Sprechstunde für Erwachsene
Kerstin Mörke/
Anja Lübbers
Ambulanzassistentinnen
0761 270-37500
0761 270-77650
Sprechstunde für Kinder
Henrike Ritterbusch
Kinderkrankenschwester
0761 270-45240