Vaskuläre Biologie
Projektleiter: Prof. Dr. Sebastian Grundmann
The main research focus of our laboratory group is the investigation and characterization of small non-coding regulatory RNA molecules in cardiovascular processes and diseases. We address a broad field of cardiovascular research areas such as chronic vascular inflammation, ischemia/reperfusion injury, in-stent restenosis, blood vessel growth as well as metabolic disorders, which are all strongly connected with arterial occlusive diseases. Our goal is to elucidate the role of regulatory RNAs in the underlying mechanism of these disease processes, with the ultimate aim to contribute to the development of new pharmacological strategies based on microRNA-substitution or inhibition for the treatment of vascular occlusive diseases.

Prof. Dr. med. Sebastian Grundmann
Lab head, Principle Investigator
Telefon: +49 761 270-70460
Telefax: +49 761 270-70450
E-Mail: sebastian.grundmann@uniklinik-freiburg.de

Dr. rer. nat. Franziska Pankratz
Co-lab head, Principal Investigator
Tel.: +49 (0)761 270 70460
Fax: +49 (0)761 270 70450
E-Mail: franziska.pankratz@uniklinik-freiburg.de

Dr. rer. nat. Christian Smolka
Postdoc

Dipl. Biol. Caterina Jänich
Technican

Alexander Asmussen
Research Fellow, Cardiology

Xavier Bemtgen
Research Fellow, Cardiology

Catherine Hohnloser
Research Fellow, Cardiology

Maike Bach
Veterinarian

Julien Martin
Medical Student

Laura Anna Schneider
Medical Student
In the past decade, a new class of gene expression regulators has emerged: microRNAs. These small non-coding RNAS regulate gene expression on a post-transcriptional level and one microRNA is able to regulate several independent or functionally related mRNA target genes, thereby modulating broad range of biological processes and pathological disorders. Our focus in this research area lies on microRNA function in cardiovascular occlusive diseases and we develop new therapeutic strategies for cardial protection and healing based on either microRNA substitution or inhibition.
MicroRNAs in chronic vascular inflammation
Vascular inflammation is not only a critical component of the host –defense reaction against external pathogens and injury, but also an important modulator of pathological conditions such as atherosclerotic lesion formation. We are interested in the function of microRNAs in processes relevant for chronic vascular inflammation such as endothelial-leukocyte interaction, homing and migration of immune cells and their modulation of pro- as well as anti-inflammatory signaling cascades. We also investigate the impact of either microRNA inhibition or overexpression on atherosclerotic lesion formation and the plaque phenotype.
MicroRNAs in ischemia-reperfusion injury
Ischemia-reperfusion injury is the term for a harmful inflammatory process occurring during restoration of blood flow following a critical time of ischemia. I/R-injury plays an important role in different clinical setting such as myocardial infarction, stroke as well as transplant surgery. Ischemia-reperfusion is determined by different components such as the infiltration of circulating cells in the injured tissue and the local generation of reactive oxygen species. We investigate the role of microRNAs in ischemia-reperfusion injury using two different in vivo models: temporary occlusion of the left anterior descending artery for induction of myocardial infarction in the mouse heart and the preparation of the cremaster muscle to allow the in vivo imaging of endothelial-leukocyte interaction. Both models combined with histological and gene expression analysis are used for the characterization of microRNAs in the process of harmful and protective mechanisms during ischemia and reperfusion.

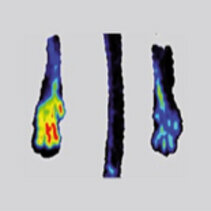
MicroRNAs in in stent-restenosis and arterial remodelling
Restenosis describes the narrowing or occlusion of a blood vessel for example following coronary stent implantation and it is caused by a proliferation of vascular smooth muscle cells (VSMC) into the lumen. VSMCs control the organisms` circulatory homeostasis by regulating the tone of arteries and arterioles and can switch between two phenotypes: contractile and synthetic. The latter is a critical part of embryonic and fetal development as well as physiological adaption to pregnancy and exercise, but can also be a harmful response to vascular injury due to atherosclerosis, hypertension or percutaneous coronary interventions. We investigate the impact of microRNAs on the phenotype switch of VSMCs in vitro as well as on neointima formation in vivo.

MicroRNAs in energy metabolism
In industrial countries, the number of people developing a metabolic syndrome is rapidly increasing and is mainly caused by an unfavorable lifestyle in combination with genetic predispositions. In the last years, microRNAs came into the focus in this area of research and so far several microRNAs have been reported to be involved in the regulation of metabolic processes. Our group focuses on the investigation of microRNAs in the regulation of key metabolic mRNAs and their proteins and our goal is to define their function in the development of age related diseases like diabetes and obesity.
MicroRNAs and adaptive neovascularization
The adaptive growth of arteries is an important protective mechanism in patients with vascular occlusive disease. We investigate the molecular mechanisms regulating this process and attempt to stimulate the growth of capillaries and collateral arteries as a possible future therapeutic approach. Angiogenesis (the growth of capillaries) and arteriogenesis (the growth of arteries) involves the complex interactions of different cell types, including endothelial cells, smooth muscle cells and circulating cells, especially infiltrating monocytes and macrophages. We are especially interested in the use of microRNA therapeutic to stimulate pro-arteriogenic processed without unwanted side effects on angiogenic tumor growth.
First transfemoral percutaneous edge-to-edge repair of the tricuspid valve using the MitraClip system.
Wengenmayer T, Zehender M, Bothe W, Bode C, Grundmann S.
EuroIntervention. 2016 Apr 20;11(13):1541-4.
Response to Letter Regarding Article, "MicroRNA-155 Exerts Cell-Specific Antiangiogenic but Proarteriogenic Effects During Adaptive Neovascularization".
Pankratz F, Bemtgen X, Zeiser R, Leonhardt F, Kreuzaler S, Hilgendorf I, Smolka C, Helbing T, Hoefer I, Esser JS, Kustermann M, Moser M, Bode C, Grundmann S.
Circulation. 2015 Dec 8;132(23):e376.
MicroRNA-155-deficient dendritic cells cause less severe GVHD through reduced migration and defective inflammasome activation.
Chen S, Smith BA, Iype J, Prestipino A, Pfeifer D, Grundmann S, Schmitt-Graeff A, Idzko M, Beck Y, Prinz G, Finke J, Duyster J, Zeiser R.
Blood. 2015 Jul 2;126(1):103-12
MicroRNA-132/212 family enhances arteriogenesis after hindlimb ischemia through modulation of the Ras-MAPK pathway.
Lei Z, van Mil A, Brandt MM, Grundmann S, Hoefer I, Smits M, El Azzouzi H, Fukao T, Cheng C, Doevendans PA, Sluijter JP.
J Cell Mol Med. 2015 Aug;19(8):1994-2005.
MicroRNA-155 modulates P2R signaling and Th2 priming of dendritic cells during allergic airway inflammation in mice.
Zech A, Ayata CK, Pankratz F, Meyer A, Baudiß K, Cicko S, Yegutkin GG, Grundmann S, Idzko M.
Allergy. 2015 Sep;70(9):1121-9.
MicroRNA-155 aggravates ischemia-reperfusion injury by modulation of inflammatory cell recruitment and the respiratory oxi dative burst.
Eisenhardt SU, Weiss JB, Smolka C, Maxeiner J, Pankratz F, Bemtgen X, Kustermann M, Thiele JR, Schmidt Y, Bjoern Stark G, Moser M, Bode C, Grundmann S.
Basic Res Cardiol. 2015 May;110(3):32.
MicroRNA-155 Exerts Cell-Specific Antiangiogenic but Proarteriogenic Effects During Adaptive Neovascularization.
Pankratz F, Bemtgen X, Zeiser R, Leonhardt F, Kreuzaler S, Hilgendorf I, Smolka C, Helbing T, Hoefer I, Esser JS, Kustermann M, Moser M, Bode C, Grundmann S.
Circulation. 2015 May 5;131(18):1575-89.
The transcription factor HoxB5 stimulates vascular remodelling in a cytokine-dependent manner.
Fessner A, Esser JS, Bluhm F, Grundmann S, Zhou Q, Patterson C, Bode C, Moser M.
Cardiovasc Res. 2014 Feb 1;101(2):247-55.
FoxP1 stimulates angiogenesis by repressing the inhibitory guidance protein semaphorin 5B in endothelial cells.
Grundmann S, Lindmayer C, Hans FP, Hoefer I, Helbing T, Pasterkamp G, Bode C, de Kleijn D, Moser M.
PLoS One. 2013 Sep 2;8(9):e70873
Inhibition of BMP activity protects epithelial barrier function in lung injury.
Helbing T, Herold EM, Hornstein A, Wintrich S, Heinke J, Grundmann S, Patterson C, Bode C, Moser M.
J Pathol. 2013 Sep;231(1):105-16
CD26 inhibition enhances perfusion recovery in ApoE-/-mice.
Haverslag RT, de Groot D, Grundmann S, Meder B, Goumans MJ, Pasterkamp G, Hoefer IE, de Kleijn DP.
Curr Vasc Pharmacol. 2013 Jan;11(1):21-8
Distinct CD44 splice variants differentially affect collateral artery growth.
Bot PT, Grundmann S, van Royen N, Joosten SP, Schirmer SH, de Kleijn DP, Pals ST, Pasterkamp G, Piek JJ, Hoefer IE.
Curr Vasc Pharmacol. 2013 Jan;11(1):13-20.
Inflammatory neovascularization during graft-versus-host disease is regulated by αv integrin and miR -100.
Leonhardt F, Grundmann S, Behe M, Bluhm F, Dumont RA, Braun F, Fani M, Riesner K, Prinz G, Hechinger AK, Gerlach UV, Dierbach H, Penack O, Schmitt-Gräff A, Finke J, Weber WA, Zeiser R.
Blood. 2013 Apr 25;121(17):3307-18.
MicroRNAs in ischemia-reperfusion injury.
Weiss JB, Eisenhardt SU, Stark GB, Bode C, Moser M, Grundmann S.
Am J Cardiovasc Dis. 2012;2(3):237-47. Epub 2012 Jul 25.
Perturbation of the endothelial glycocalyx in post cardiac arrest syndrome.
Grundmann S, Fink K, Rabadzhieva L, Bourgeois N, Schwab T, Moser M, Bode C, Busch HJ.
Resuscitation. 2012 Jun;83(6):715-20
MicroRNA-214 inhibits angiogenesis by targeting Quaking and reducing angiogenic growth factor release.
van Mil A, Grundmann S, Goumans MJ, Lei Z, Oerlemans MI, Jaksani S, Doevendans PA, Sluijter JP.
Cardiovasc Res. 2012 Mar 15;93(4):655-65.
BMP activity controlled by BMPER regulates the proinflammatory phenotype of endothelium.
Helbing T, Rothweiler R, Ketterer E, Goetz L, Heinke J, Grundmann S, Duerschmied D, Patterson C, Bode C, Moser M.
Blood. 2011 Nov 3;118(18):5040-9.
Forkhead box protein P1 as a downstream target of transforming growth factor-β induces collagen synthesis a nd correlates with a more stable plaque phenotype.
Bot PT, Grundmann S, Goumans MJ, de Kleijn D, Moll F, de Boer O, van der Wal AC, van Soest A, de Vries JP, van Royen N, Piek JJ, Pasterkamp G, Hoefer IE.
Atherosclerosis. 2011 Sep;218(1):33-43
MicroRNA-100 regulates neovascularization by suppression of mammalian target of rapamycin in endothelial and vascular smooth muscle cells.
Grundmann S, Hans FP, Kinniry S, Heinke J, Helbing T, Bluhm F, Sluijter JP, Hoefer I, Pasterkamp G, Bode C, Moser M.
Circulation. 2011 Mar 8;123(9):999-1009.
Inflammasome activation in reperfusion injury: friendly fire on myocardial infarction?
Grundmann S, Bode C, Moser M.
Circulation. 2011 Feb 15;123(6):574-6.
MicroRNA regulation of angiogenesis and arteriogenesis.
Hans FP, Moser M, Bode C, Grundmann S.
Trends Cardiovasc Med. 2010 Nov;20(8):253-62.
Assessment of collateral artery function and growth in a pig model of stepwise coronary occlusion.
de Groot D, Grundmann S, Timmers L, Pasterkamp G, Hoefer IE.
Am J Physiol Heart Circ Physiol. 2011 Jan;300(1):H408-14.
An ultrasound contrast agent targeted to P-selectin detects activated platelets at supra-arterial shear flow conditions.
Guenther F, von zur Muhlen C, Ferrante EA, Grundmann S, Bode C, Klibanov AL.
Invest Radiol. 2010 Oct;45(10):586-91.
Arteriogenesis requires toll-like receptor 2 and 4 expression in bone-marrow derived cells.
de Groot D, Hoefer IE, Grundmann S, Schoneveld A, Haverslag RT, van Keulen JK, Bot PT, Timmers L, Piek JJ, Pasterkamp G, de Kleijn DP.
J Mol Cell Cardiol. 2011 Jan;50(1):25-32.
Mannose-binding lectin: an ancient molecule with new implications in myocardial infarction.
Grundmann S, Bode C, Moser M.
Eur Heart J. 2010 May;31(10):1163-4.
Prosthetic valve endocarditis due to Actinomyces neuii successfully treated with antibiotic therapy.Grundmann S, Huebner J, Stuplich J, Koch A, Wu K, Geibel-Zehender A, Bode C, Brunner M.
J Clin Microbiol. 2010 Mar;48(3):1008-11.
Neurologic prognosis after cardiac arrest.
Grundmann S, Busch HJ.
N Engl J Med. 2009 Nov 12;361(20):1999; author reply 1999-2000.
Endothelial glycocalyx dimensions are reduced in growing collateral arteries and modulate leucocyte adhesion in arteriogenesi s.
Grundmann S, Schirmer SH, Hekking LH, Post JA, Ionita MG, de Groot D, van Royen N, van den Berg B, Vink H, Moser M, Bode C, de Kleijn D, Pasterkamp G, Piek JJ, Hoefer IE.
J Cell Mol Med. 2009 Sep;13(9B):3463-74.
[Cytokine-eluting stents as new drug-delivery devices for angiogenic therapy].
Grundmann S, Hoefer I, Bode C.
Hamostaseologie. 2008 Oct;28(4):195-202. Review. German.
Arteriogenesis: basic mechanisms and therapeutic stimulation.
Grundmann S, Piek JJ, Pasterkamp G, Hoefer IE.
Eur J Clin Invest. 2007 Oct;37(10):755-66.
A new intra-arterial delivery platform for pro-arteriogenic compounds to stimulate collateral artery growth via transforming growth factor-beta1 release.
Grundmann S, van Royen N, Pasterkamp G, Gonzalez N, Tijsma EJ, Piek JJ, Hoefer IE.
J Am Coll Cardiol. 2007 Jul 24;50(4):351-8.
Granulocyte-macrophage colony-stimulating factor stimulates arteriogenesis in a pig model of peripheral artery disease using clinically applicable infusion pumps.
Grundmann S, Hoefer I, Ulusans S, Bode C, Oesterle S, Tijssen JG, Piek JJ, Buschmann I, van Royen N.
J Vasc Surg. 2006 Jun;43(6):1263-9
Aspirin, but not clopidogrel, reduces collateral conductance in a rabbit model of femoral artery occlusion.
Hoefer IE, Grundmann S, Schirmer S, van Royen N, Meder B, Bode C, Piek JJ, Buschmann IR.
J Am Coll Cardiol. 2005 Sep 20;46(6):994-1001.
Leukocyte subpopulations and arteriogenesis: specific role of monocytes, lymphocytes and granulocytes.
Hoefer IE, Grundmann S, van Royen N, Voskuil M, Schirmer SH, Ulusans S, Bode C, Buschmann IR, Piek JJ. Atherosclerosis. 2005 Aug;181(2):285-93.
Anti-tumor necrosis factor-{alpha} therapies attenuate adaptive arteriogenesis in the rabbit.
Grundmann S, Hoefer I, Ulusans S, van Royen N, Schirmer SH, Ozaki CK, Bode C, Piek JJ, Buschmann I.
Am J Physiol Heart Circ Physiol. 2005 Oct;289(4):H1497-505.
Differential effects of MCP-1 and leptin on collateral flow and arteriogenesis.
Schirmer SH, Buschmann IR, Jost MM, Hoefer IE, Grundmann S, Andert JP, Ulusans S, Bode C, Piek JJ, van Royen N.
Cardiovasc Res. 2004 Nov 1;64(2):356-64.
Arteriogenesis proceeds via ICAM-1/Mac-1- mediated mechanisms.
Hoefer IE, van Royen N, Rectenwald JE, Deindl E, Hua J, Jost M, Grundmann S, Voskuil M, Ozaki CK, Piek JJ, Buschmann IR.
Circ Res. 2004 May 14;94(9):1179-85.
Invasive and non-invasive evaluation of spontaneous arteriogenesis in a novel porcine model for peripheral arterial obstructive disease.
Buschmann IR, Voskuil M, van Royen N, Hoefer IE, Scheffler K, Grundmann S, Hennig J, Schaper W, Bode C, Piek JJ.
Atherosclerosis. 2003 Mar;167(1):33-43.
Local monocyte chemoattractant protein-1 therapy increases collateral artery formation in apolipoprotein E-deficient mice but induces systemic monocytic CD11b expression, neointimal formation, and plaque progression.
van Royen N, Hoefer I, Böttinger M, Hua J, Grundmann S, Voskuil M, Bode C, Schaper W, Buschmann I, Piek JJ.
Circ Res. 2003 Feb 7;92(2):218-25.
Labor

Prof. Dr. med. Sebastian Grundmann
Lab head, Principle Investigator
Telefon: +49 761 270-70460
Telefax: +49 761 270-70450
E-Mail: sebastian.grundmann@uniklinik-freiburg.de


