Translational Cardiovascular Outcomes Research
Who we are
We are a junior group of clinician-scientists committed to improving outcomes of patients with cardiovascular disease by integrating experimental and clinical research with data and biomaterial repositories. We foster flat hierarchies, open communication and collaborative decision-making.
Research areas
Cardiogenic Shock
Cardiogenic Shock (CS) is a life-threatening condition with high short- and long-term mortality and morbidity. With the multi-center MIRACLE study, we aim to refine outcome prediction and gain mechanistic insights - both for acute in-hospital outcomes and to understand how specific phenotypes and treatment characteristics shape long-term residual mortality, morbidity, and quality of life. Extensive biobanking during hospitalization and at follow-up supports future research.
Cardio-Obstetrics
Hypertensive Disorders of Pregnancy (HDP) are a major cause of maternal morbidity and are strongly linked to future cardiovascular disease. Through TWILIGHT, we aim to leverage pregnancy as a predictive window for cardiovascular health by integrating gestational outcomes and blood samples collected during pregnancy with individual long-term data from the Danish National Patient Registry. We are further interested in cardiovascular biomarkers during gestation and their value for HDP prediction.
Pregnancy in women with cardiac disease: Managing pregnancy in women with congenital or acquired heart disease requires specialized interdisciplinary care. With the PRECARD study we aim to refine risk stratification and assess long-term patient-centered outcomes in this population.
Team

Dr. Lucas Bacmeister
Lead (TWILIGHT; ARCTIC), Co-Lead (MIRACLE; PRECARD)

Dr. Adrian Heidenreich
Co-Lead (MIRACLE)

Dr. Annette Büllesbach
Co-Lead (PRECARD; MIRACLE)

Leonie Ziegler
Investigator (MIRACLE)

Jonas Hein
Investigator (MIRACLE)

Sebastian König
Investigator (MIRACLE)
sebastian.koenig@uniklinik-freiburg.de

Dr. Philipp Albrecht
Investigator (MIRACLE)
Niklas Hempfling
Investigator (ARCTIC)

Marion Klima
Study Nurse

Luca Rappold
MD student (MIRACLE)

Philipp Domke
MD student (MIRACLE)

Leonie Walz
MD student (MIRACLE)

Jakob Madlinger
MD student (MIRACLE)

Mirjam Paul
MD student (PRECARD)

Stefanie Kleeb
MD student (PRECARD)

Debora Ehrhardt
Student researcher (TWILIGHT)
Project updates:
Current enrollment status of the MIRACLE study.
Cardiogenic shock (CS) is a life-threatening condition characterized by a severe reduction in cardiac output, leading to systemic hypoperfusion, multiorgan failure, and a mortality rate exceeding 30% in hospitalized patients. The primary causes of CS are acute myocardial infarction (AMI) and acutely decompensated heart failure (ADHF), though secondary CS resulting from arrhythmias, valvular dysfunction, right ventricular failure, and septic overlap are increasingly recognized. Beyond the immediate risk of acute mortality, many CS survivors face significant long-term morbidity and an elevated risk of mortality.
To enhance precision phenotyping and risk stratification, we designed the MIRACLE study, a multi-center, prospective, longitudinal cohort study. Our goal is to enable a comprehensive characterization and follow-up of CS patients across all etiologies and severities (SCAI classifications B to E). With a substudy, MIRACLE-SurvivorS, we specifically focus on CS survivors, tracking patient reported outcomes and clinical endpoints longitudinally through the first year.
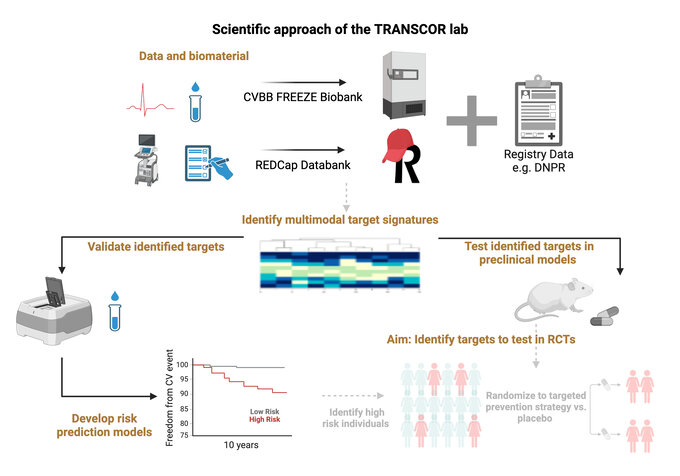
Biobanking is conducted in collaboration with the Cardiovascular Biobank (CVBB), a hub of the FREEZE-Biobank, during both the acute phase and the long-term follow-up. Thereby, we aim to understand how molecular pathways drive differential recovery from CS.
MIRACLE has received start-up funding from the Programm Klinische Studien of the Medical Faculty of the University of Freiburg and from the Else Kröner-Fresenius-Foundation. It is registered at the Deutsches Register Klinischer Studien.
Project updates:
Recent findings have been published in Circulation and JACC:Advances
Pregnancy acts as a cardiovascular stress test. Hypertensive disorders of pregnancy (HDPs), including conditions such as preeclampsia, are major causes of maternal morbidity and are strongly linked to an increased risk of future cardiovascular disease. While many studies have demonstrated this association, the underlying causal mechanisms remain unclear, and there is limited understanding of the specific biomarkers and phenotypes during pregnancy that may predict premature cardiovascular disease in women—an area that has not received the attention it deserves until recently.
Through the TWILIGHT project, we aim to leverage pregnancy as an early window to predict short- and long-term cardiovascular health in women. In collaboration with Professor Marianne Andersen, a co-founder of the Danish Odense Child Cohort, and Professor Ralf Dechend, Charité Berlin, we are studying women who were pregnant between 2010 and 2012. By integrating data on their pregnancy outcomes and blood samples drawn during gestation with long-term health data from the The Danish National Patient Register, our goal is to identify biomarkers and mechanisms that may contribute to premature cardiovascular disease in women. We aim to translate these findings into targeted prevention strategies that can be implemented directly postpartum, providing early interventions for women at very high cardiovascular risk.
Project updates:
The PRECARD registry evaluates both clinical outcomes and the long-term cardiovascular impact of pregnancies in women with congenital or acquired heart disease, receiving interdisciplinary care at University Hospital Freiburg. It also explores the perceptions during pregnancy of this patient population, including their experience with care, expectations, and the teamwork among treating physicians, as well as their long-term quality of life. The primary aim is to understand how to improve care and outcomes for this population, with findings guiding future approaches to interdisciplinary patient management.
Project updates: Preliminary findings have been presented at the 9th International Congress on Cardiac Problems in Pregnancy (CPP 2025) and the German Cardiac Society’s annual congress in 2025.
Project updates:
Recent findings have been published in Circulation: Cardiovascular Imaging
Immune checkpoint inhibitors (ICIs) have revolutionized cancer treatment by enhancing antitumor T-cell activity, leading to significant improvements in outcomes across various cancers. Over the past decade, eligibility for ICI therapy has expanded rapidly. However, concerns about the cardiovascular risks of ICIs have emerged, particularly the potential for accelerated vascular atherosclerosis. ICIs may trigger T-cell autoreactivity against autoantigens, leading to arterial inflammation and an increased risk of long-term cardiovascular events in treated patients.
The ARCTIC project aims to investigate the ability of arterial arterial 2-deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) uptake in routine staging positron emission tomography (PET) scans to detect arterial inflammation in cancer patients treated with ICIs. By comparing changes in arterial tracer uptake between ICI-treated patients and non-treated controls across repeated scans, our goal is to assess the impact of ICIs on arterial inflammation and to better understand the mechanisms by which ICIs may increase atherosclerosis.
ARCTIC is a collaborative effort with PD Dr. Dr. Christian Goetz from the Department of Nuclear Medicine and Prof. Dr. Dennis Wolf from the Vascular Immunology Lab.
Collaborators at the University of Freiburg
Christian Goetz, Department of Nuclear Medicine (ARCTIC)
Sebastian Grundmann, UHC (PRECARD)
Till Keller, UHC, Data management and biobanking (MIRACLE)
Diana Lindner, UHC, Molecular Cardiology lab (TWILIGHT, MIRACLE)
Alexander Maier, UHC, Interventional Cardiology and Imaging lab (ARCTIC)
Christoph Olivier, UHC, Cardiovascular Clinical Research Center (MIRACLE)
Susanne Weber / Klaus Kaier, Medical Biometry and Statistics
Tobias Wengenmayer, Interdisciplinary Intensive Care (MIRACLE)
Dirk Westermann, UHC (TWILIGHT, MIRACLE)
Dennis Wolf, UHC, Vascular Immunology lab (ARCTIC)
External collaborators
Marianne Skovsager Andersen, University of Southern Denmark, Odense (TWILIGHT)
Ralf Dechend, Charité und Max-Delbrück Center, Berlin (TWILIGHT)
Sebastian Ewen, SBK Villingen-Schwenningen (MIRACLE)
Jan Stener Jørgensen, University of Southern Denmark, Odense (TWILIGHT)
Matthias Pauschinger, Paracelsus-Universitätsklinikum Nürnberg (MIRACLE)
Ulrich Pecks, University of Würzburg (TWILIGHT)
Christina Anne Vinter, University of Southern Denmark, Odense (TWILIGHT)
Tanja Zeller, University of Lübeck (TWILIGHT)
Third-Trimester NT-proBNP for Pre-eclampsia Risk Prediction: A Comparison with sFlt-1/PlGF in a Population-Based Cohort; JACC:Advances, 2025
Bacmeister, L, …, Buellesbach, A, …, Heidenreich, A,… Andersen, M*, Dechend, R*, Westermann, D*
Longitudinal Assessment of Subclinical Arterial Inflammation in Patients Receiving Immune Checkpoint Inhibitors by Sequential [18F]FDG PET Scans; Circulation:Cardiovasc Imaging, 2025
Bacmeister, L, Hempfling, N, …, Buellesbach, A, Heidenreich, A, …, Wolf, D
Man versus machine in advanced heart failure: Can AI beat clinicians?; Eur J Heart Fail, 2025
Bacmeister, L, Codina, P, Westermann, D
High-Sensitivity Cardiac Troponin I Enhances Preeclampsia Prediction Beyond Maternal Factors and the sFlt-1/PlGF Ratio; Circulation, 2024
Bacmeister, L, … Buellesbach, A, ... Dechend, R*, Westermann, D*, Zeller, T*
P2X7 Deficiency Blocks Lesional Inflammasome Activity and Ameliorates Atherosclerosis in Mice; Circulation, 2017
Stachon, P*, Heidenreich, A*, …, Idzko, M*, Zirlik, A*