Research
Center for Excellence "Fragile Skin"

Emeriti:
Prof. Dr. Dr. h.c. Leena Bruckner-Tuderman, MD
E-mail: leena.bruckner-tuderman[at]uniklinik-freiburg.de
Phone: +49 (0)761 270-67160
The Center of Excellence “Fragile Skin” combines clinical patient care, molecular diagnostics and experimental research. The term “Fragile Skin” was coined for disorders of the skin and mucous membranes, which manifest with blister formation, easy bruisability or tearing, slow or disturbed wound healing, and reduced resistance against external mechanical forces. The Center is hosted by the Department of Dermatology, Medical Center - University of Freiburg. Its functions are based on intensive interactions of research and clinical medicine and encompass the following:
- high standards in interdisciplinary medical care and nursing
- modern molecular diagnostics of skin fragility disorders
- internationally competitive experimental research
- development of novel molecular and cellular therapeutic strategies.
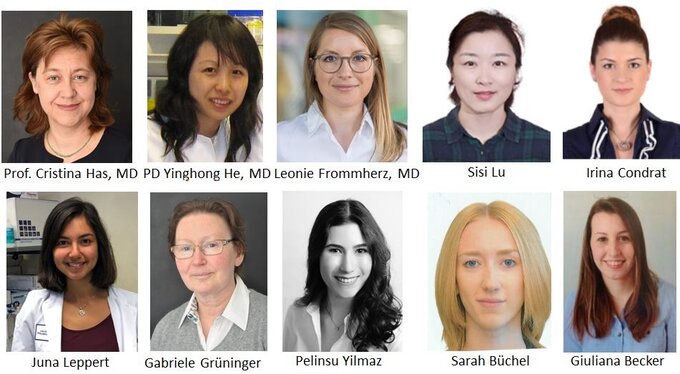
The lab members are an international group comming from Germany, Finland, France, Greece, Romania, Sweden, China, and India. The center participates in several international networks for basic and clinical research. Below, the different areas of research in the center are introduced:
Molecular basis of skin fragility and mechanisms of genetic skin fragility associated with anomalies of proteins of focal adhesions

Prof. Dr. Cristina Has, MD
E-mail: cristina.has[at]uniklinik-freiburg.de
Phone: +49 (0)761 270-67850
Dr. Yinghong He, MD
Awardee of the Else Kröner-Fresenius-Stiftung
E-mail: yinghong.he[at]uniklinik-freiburg.de
Phone:+49 (0)761 270-67210
Our group was involved in the identification of new genes for genetic skin fragility disorders - the Kindler syndrome, the acantholytic epidermolysis bullosa and junctional epidermolysis bullosa with renal and respiratory involvement. We have characterized large cohorts of patients with different types of epidermolysis bullosa, established genotype-phenotype correlations and explored the underlying disease mechanisms. In particular, we aim to understand the molecular mechanisms of disorders due to genetic defects of proteins associated with focal adhesions, kindlin-1 and the integrin a3 subunit, and the interactions between kindlins in the skin.
Former members: Dr. Anja Heinemann, PhD; Dr. Corinna Herz, PhD; Dr. Johannes S. Kern, MD, PhD; Prof. Dr. Dimitra Kiritsi, MD; Dr. Kristin Maier; Dr. Chiara Pazzagli, PhD; Dr. Manuela Pigors, PhD; Dr. Elena Zimina PhD

Prof. Dr. Dimitra Kiritsi, MD
Group leader
E-mail: dimitra.kiritsi[at]uniklinik-freiburg.de
Phone: +49 (0)761 270-67401
Career path
- Habilitation (Privatdozent), Postzygotic mosaicism in genetic skin disorders: causes and pathogenetic mechanisms, University of Freiburg
- Fellow of the European Board of Dermatology & Venereology (FEBDV) and Board Exam. Dermatology, Germany
- Group Leader, Dpt of Dermatology, Medical Center – University of Freiburg, Germany
- Postdoctoral Fellow, L. Bruckner-Tuderman laboratory, Dpt of Dermatology, Medical Center - University of Freiburg, Germany
- Thesis (Dr. med.), Molecular basis and phenotypic variability in hereditary skin fragility syndromes, L. Bruckner-Tuderman laboratory, Dpt of Dermatology, Medical Center- University of Freiburg, Germany
- MD, Kapodistriakon and Ethnikon University of Athens, Greece
Our work focuses on characterizing the causes and pathogenetic mechanisms of genetic and acquired causes of skin fragility. We focus on gaining a better understanding of how skin fragility disorders arise and especially the connection to inflammation, the immune system and the development of skin carcinomas. A special interest exists on the genetic skin disorder epidermolysis bullosa, for which we are investigating disease modifiers and how they change disease progression and attempt to identify biomarkers. Using patient material and animal models we are examining the therapeutic potential of novel treatment options, e.g. mesenchymal stem cells or “revertant mosaic” cells. In terms of autoimmune skin fragility disorders, our group is involved in the characterization of rare subtypes, enabling establishment of diagnostic algorithms and therapeutic regimes. Further, pathogenetic causes of poor wound healing are being investigated, both in genetic models, but also using cells of individuals with common causes of leg ulcers. By leading several clinical trials, direct transfer from the work on the bench to the bedside is facilitated.
Our group combines clinical expertise and laboratory research with the goal of disclosing pathogenetic disease mechanisms resulting in skin fragility, promoting the understanding of disease variability, and improving the diagnostic and therapeutic possibilities for skin fragility diseases, either genetic or acquired. Our research is funded by the German Research Foundation (CRC1160, CRC1479, other DFG grants), EB Research Partnership (USA), the Fritz-Thyssen Foundation, the Berta-Ottenstein programme for Advanced Clinician Scientists, as well as the industry. In addition, Prof. Dr. Kiritsi's work has received several awards and scholarships.
Please find current publications here

Dr. Alexander Nyström, PhD
Group leader
E-mail: alexander.nystroem[at]uniklinik-freiburg.de
Phone: +49 (0)761 270 67850
Career
- Group leader, Molecular dermatology lab, Dpt of Dermatology, Medical Center – University of Freiburg, Germany
- Postdoc, L. Bruckner-Tuderman laboratory, Dpt of Dermatology, Medical Center – University of Freiburg, Germany
- Postdoc, Renato Iozzo laboratory, Thomas Jefferson University, Philadelphia, PA, USA
- PhD in Developmental biology at Lund University, Lund, Sweden
The extracellular matrix is essential for multicellular life; it provides structure and instructions to organ systems and tissues of all phases – developing, regenerative and homeostatic. Naturally, changes in the extracellular matrix can be a catalyst of disease. Our translational research is focused on dissecting the roles of the extracellular matrix in skin during homeostasis, normal and pathological wound healing, immune surveillance and in cancer. We use this knowledge to develop new therapy approaches for treatment of bacterial infections, fibrosis and squamous cell carcinoma. A specific interest is on improving the understanding of disease mechanisms in the genetic skin blistering disease, dystrophic epidermolysis bullosa, toward developing safe, efficacious targeted-treatment.
Our research is and has been funded by national and international grants, including grants from the German Research Foundation (Deutsche Forschungsgemeinschaft), the Federal Ministry of Education and Research (Bundesministeriums für Bildung und Forschung), Dystrophic Epidermolysis Bullosa Research Association (DEBRA) and through collaboration with industry partners. We are currently part of several collaborative research centers (CRCs) – CRC850, CRC1160 and CRC1479.
Please find current publications here

Prof. Dr. Cassian Sitaru, MD
E-mail: cassian.sitaru[at]uniklinik-freiburg.de
Phone: +49 (0)761 270-69920
Helper T (Th) cell-regulated development of antigen-specific B and plasma cells resulting in the production of pathogenic autoantibodies underpins the pathology of several autoimmune diseases. These include pemphigus, pemphigoid, myasthenia gravis, Guillan-Barre syndrome, autoimmune hemolytic anemia, immune thrombocytopenia, autoimmune dilative cardiomyopathy, Goodpasture’s syndrome, systemic lupus erythematosus, anti-phospholipid syndrome, and rheumatoid arthritis. Our research focuses on the mechanisms governing the coupling of autoantibody specificity to effector cell response, with special emphasis on autoantibodies against structural skin proteins in autoimmune blistering diseases. These diseases are clinically and immunopathologically well-defined entities where both the autoantigen and the pathogenic autoantibodies are well characterized. However, the complex pathogenic and regulatory mechanisms of pathogenic autoantibody production and several aspects of blister formation are still poorly understood. A major focus of our research is to investigate these pathogenetic mechanisms using in vitro and in vivo models of autoimmunity against structural skin proteins. In parallel projects, we study the structure and function of skin proteins, including collagens VII and XVII of the dermoepidermal junction such as collagen XVII (BP180) or p200, which are targets of the autoimmune response in a group of acquired blistering diseases. Ongoing patient-centered studies address the pathogenesis of pemphigus, a severe bullous dermatosis with intraepidermal blistering, with the aim of improving diagnosis and therapy.
